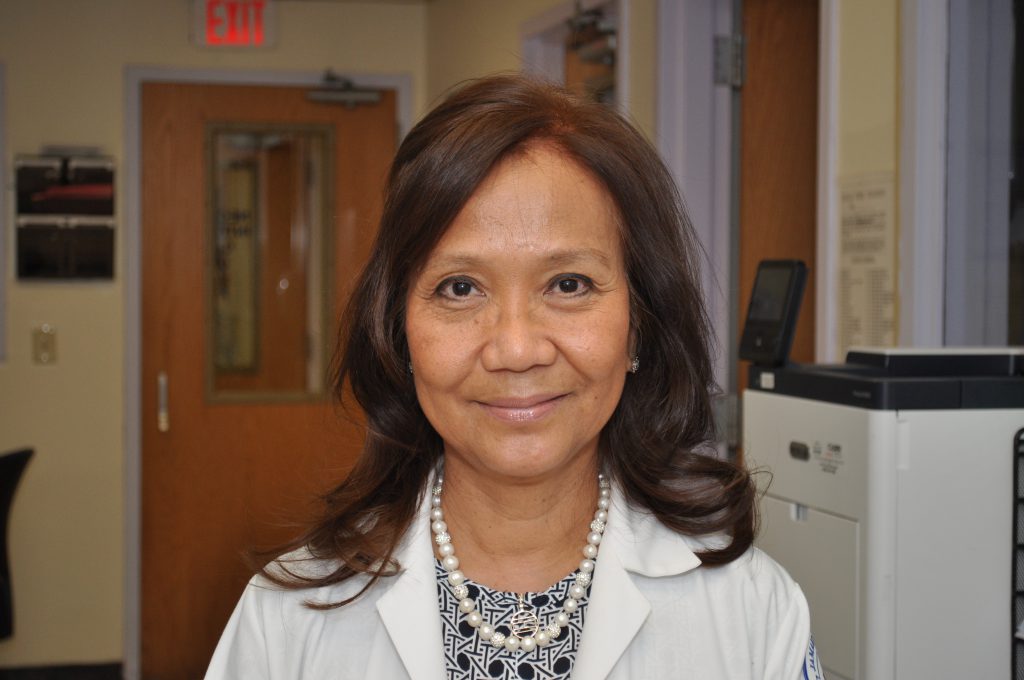
This month, we are proud to shine our Employee Spotlight on Eulanda Corales, DNP, RN, CCRN, Clinical Nurse Manager for the NICU and Pediatric unit.
Eulanda has been at Jamaica Hospital Medical Center for 36 years. She grew up in the Philippines where she attended elementary school, high school and obtained her RN degree. She moved to Queens in 1986 and has since obtained her Master’s degree in Nursing Administration at Adelphi University and her Doctorate degree from Chamberlain University. Eulanda now resides on Long Island.
Eulanda has two daughters who are both nurses and that she is very proud of. Her older daughter is a NICU nurse and her younger daughter is a Pediatric Cardiothoracic ICU nurse. She also has a granddaughter who is one year and nine months old. Her granddaughter brings her much joy and she loves spending time with her. Her granddaughter’s favorite thing to do is to dance and sing, especially to Michael Buble’s version of the song “Sway” and “Save the Last Dance for Me”.
In her free time, Eulanda enjoys reading and online window shopping. She likes many types of sports, especially archery, volleyball, rock climbing, jet skiing, parasailing, standup paddling, and body paddling. Eulanda enjoys travelling and has been to many places of interest that include all of the Hawaiian Islands, California, many cities in Mexico, the Bahamas, Virginia Beach, Bahrain, Kuwait and Saudi Arabia. She likes to go “Glamping” which is glamorous camping whenever she can. Eulanda also practices Neurobics which is aerobics for the brain.
Eulanda likes all types of food, especially, Indian, Mexican and Italian. While she enjoys many types of music, at the moment her favorite musician is the Croatian cellist Hauser. Her hobbies include photography, collecting stamps and coins from all over the world, and she also collects pens and beautiful rocks that she gives as gifts to her daughters at Christmas.
Eulanda enjoys working at Jamaica Hospital because everyone works well together as a team. She enjoys the diversity of the patients as well as the staff. She has learned many life lessons from the diversity of the people she has had the pleasure to meet over the years. We are very happy to have Eulanda as a member of our team and look forward to her continuing to work at the hospital for many more years.
All content of this newsletter is intended for general information purposes only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.