Testosterone is a hormone produced primarily in the testicles. It helps maintain men’s:
Testosterone is a hormone produced primarily in the testicles. It helps maintain men’s:
- Bone density
- Fat distribution
- Muscle strength and mass
- Facial and body hair
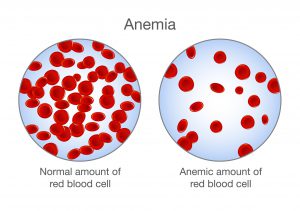
- Red blood cell production
- Sex drive
- Sperm production
Testosterone levels generally peak during adolescence and early adulthood. As you age, your testosterone level gradually declines—typically about 1% a year after turning 30 or 40 years old. For older men, it’s important to determine if a low testosterone level is due to normal aging or if it is due to a disease called hypogonadism.
Hypogonadism hampers the ability to produce normal amounts of testosterone due to a problem with the testicles or with the pituitary gland that controls the testicles. Testosterone replacement therapy, in the form of injections, pellets, patches, or gels, can improve the signs and symptoms of low testosterone in these men.
Men can have many signs and symptoms as they age. Some that might occur as a result of lower testosterone levels can include:
- Changes in sexual function
- Physical changes
- Emotional changes
Other factors, including medication side effects, obstructive sleep apnea, thyroid problems, diabetes, and depression can cause some of these signs and symptoms.
Testosterone therapy can help reverse the effects of hypogonadism, however, it is unclear whether testosterone therapy would benefit older men who are otherwise healthy. Although some men believe they feel younger and more vigorous if they take testosterone medications, there is little evidence to support the use of testosterone in otherwise healthy men. Guidelines from the American College of Physicians indicate that testosterone therapy might improve sexual function in some men, however, there is little evidence that it improves other functions, such as energy and vitality.
Testosterone therapy has various risks, including:
- Worsening sleep apnea
- Causing acne or other skin reactions
- Stimulating noncancerous growth of the prostate and growth of existing prostate cancer
- Enlarging breasts
- Limiting sperm production or causing testicles to shrink
- Stimulating too much red blood cell production contributes to an increased risk of forming a blood clot, which could cause a pulmonary embolism
If you wonder whether testosterone therapy is right for you, discuss the risks and benefits with your doctor. A blood test is used to diagnose a low testosterone. Your doctor will likely measure your testosterone levels at least twice before recommending testosterone therapy.
Treating normal aging with testosterone therapy is not advisable. If you don’t have a medical condition that is contributing to your decline in testosterone levels, your doctor might suggest natural ways to boost testosterone.
If you would like to learn more about testosterone replacement therapy, you can call and make an appointment with Jamaica Hospital’s endocrinology service, at 718-206-7001.
All content of this newsletter is intended for general information purposes only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.
 As the fall temperatures get colder we’ll be spending more time indoors. Here is a comforting fall recipe for Mom’s lasagna to keep you warm during the cold, autumn months.
As the fall temperatures get colder we’ll be spending more time indoors. Here is a comforting fall recipe for Mom’s lasagna to keep you warm during the cold, autumn months.