Peripheral neuropathy is any condition that involves damage to peripheral nerves outside your brain or spinal cord. These conditions often cause weakness, numbness, and pain, usually in the hands and feet, but can also affect other areas and body functions like digestion and urination.
Peripheral neuropathy is any condition that involves damage to peripheral nerves outside your brain or spinal cord. These conditions often cause weakness, numbness, and pain, usually in the hands and feet, but can also affect other areas and body functions like digestion and urination.
The peripheral nervous system sends information from the brain and spinal cord to the rest of the body through motor nerves. The peripheral nerves also send sensory information to the central nervous system through sensory nerves.
The nerves in the peripheral nervous system are divided into three categories and have a specific job.
- Sensory nerves that receive sensation, such as temperature, pain, vibration, or touch, from the skin
- Motor nerves that control muscle movement
- Autonomic nerves that control functions such as blood pressure, sweating, heart rate, digestion, and bladder function
Symptoms of peripheral neuropathy depend on the nerve affected and can include:
- Gradual onset of numbness, prickling, or tingling in your hands and feet. These sensations can spread upward into your arms and legs
- Sharp, jabbing, throbbing, or burning pain
- Extreme sensitivity to touch
- Pain during activities that shouldn’t cause pain, such as pain in your feet when putting weight on them, or when they’re under a blanket
- Lack of coordination and falling
- Muscle weakness
- Feeling as if you’re wearing gloves or socks when you’re not
- Inability to move if motor nerves are affected
- Heat intolerance
- Excessive sweating or not being able to sweat
- Bowel, bladder, or digestive problems
- Drops in blood pressure, causing dizziness or lightheadedness
Peripheral neuropathy can happen for many reasons. Some include:
- Type 2 diabetes
- Alcohol use disorder
- Vitamin and nutrient deficiencies
- Autoimmune and inflammatory conditions
- Medications and toxins
- Tumors
- Genetic conditions
- Infections
- Hansen disease (leprosy)
- Trauma and surgery
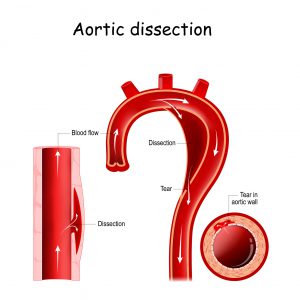
- Vascular disorders
- Idiopathic neuropathy
A combination of methods are used to diagnose peripheral neuropathy including:
- Symptoms and medical history
- Physical and neurological exams
- Lab, diagnostic, and imaging tests
Treatment of peripheral neuropathy varies depending on its cause. Treatments can include:
- Medications
- Surgery
- Physical therapy
- Devices and wearable equipment
- Podiatry and foot care
- Other pain treatments such as acupuncture, transcutaneous electrical stimulation, injections, or surgery to implant a spinal cord stimulator
Some causes of peripheral neuropathy are preventable. Some preventative or precautionary steps you can take include:
- Eating a balanced diet
- Staying physically active and maintaining a healthy weight
- Wearing safety equipment as needed
- Managing chronic conditions
- Avoiding alcohol in excess
- Avoiding exposure to toxins, poisons, and heavy metals
If you are experiencing symptoms of peripheral neuropathy, you can schedule an appointment with a doctor at Jamaica Hospital Medical Center’s Ambulatory Care Center, please call (718) 206-7001.
All content of this newsletter is intended for general information purposes only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.