Diabetes is a disease that occurs when our blood sugar or glucose is too high. This happens when the pancreas does not produce enough insulin, or can’t use insulin properly to regulate blood glucose.
Diabetes is a disease that occurs when our blood sugar or glucose is too high. This happens when the pancreas does not produce enough insulin, or can’t use insulin properly to regulate blood glucose.
Diabetes is diagnosed in a significant amount of people in our population; the Centers for Disease Control and Prevention recently reported that approximately 38.4 million people in the United States have diabetes, which is 11.6% of the population.
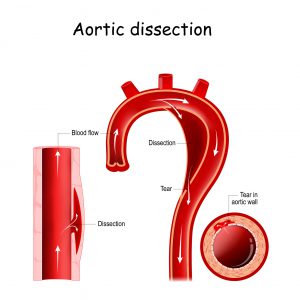
Complications such as vision loss, amputation, heart attacks, stroke, kidney disease, and even death can occur as a result of diabetes.
There is no cure for diabetes; however, the disease can be managed, and in some cases reversed through treatment and (or) healthy weight loss and lifestyle changes.
Reversing diabetes or putting it in remission means managing blood sugar levels and keeping your A1c below 48 mmol/mol or less than 6.5%, without needing to take medications for three months or more. This may be achieved by:
- Losing weight, which may help cells respond to insulin
- Exercising by doing a combination of aerobic and strength training activities
- Eating a healthy diet that is rich in lean proteins, vegetables, fruits, healthy fats and whole grains
- Avoiding foods that are high in carbohydrates
It is important to note that diabetes reversal or remission is not permanent. Therefore, there is a chance that symptoms can return. Please see your doctor right away if you are experiencing any of the following signs that are indicative of your diabetes being out of remission.
- Frequent infections
- Increased hunger, thirst, or urination
- Blurry vision
- Unexplained weight loss
- Fatigue
- Slow healing wounds
- Tingling or numbness in hands or feet
In addition, continue to see your healthcare provider regularly to ensure your diabetes is being managed well.
To schedule an appointment with a doctor at Jamaica Hospital Medical Center, please call 718-206-7001.
All content of this newsletter is intended for general information purposes only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.