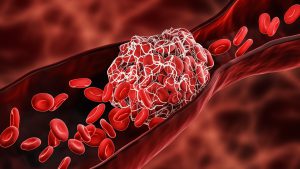
 Blood clots are gel-like clumps of blood that form in your arteries and veins. Blood clots help control bleeding, but can also cause serious medical issues like deep vein thrombosis, pulmonary embolism, and heart attack.
Blood clots are gel-like clumps of blood that form in your arteries and veins. Blood clots help control bleeding, but can also cause serious medical issues like deep vein thrombosis, pulmonary embolism, and heart attack.
Blood clots are the first line of defense if something damages your blood vessels. This is why bleeding usually stops after a few minutes when you cut yourself. You can also develop a blood clot when you have been immobile for a long time or have medical conditions that increase your risk of getting them.
Blood clots are made of small colorless fragments of cells produced by your bone marrow called platelets. They are also made of a sticky blood protein that looks like strings called fibrin. Platelets and fibrin work together to seal injured areas of your blood vessels.
You can have blood clots anywhere in your body. When they develop in the veins of your arms and legs it’s called deep vein thrombosis. Blood clots that form in the arteries of your lungs are called pulmonary embolism. A stroke occurs when blood clots block blood flow to your brain. When blood clots are in your heart, they can cause a heart attack.
If you are experiencing leg pain, swollen legs, or skin discoloration, these may be symptoms of deep vein thrombosis. Chest pain or shortness of breath can be symptoms of blood clots in your lungs or heart.
Some other possible symptoms of blood clots to be mindful of include:
- A cough that produces blood sputum
- A fast heartbeat
- Lightheadedness
- Pain that spreads to the shoulder, arm, back, or jaw
- Sudden weakness or numbness of the face, arm, or leg
- Sudden difficulty speaking or understanding speech
Some conditions focus on blood clots such as blood clotting issues. Some blood clotting disorders include:
- Factor V Leiden- an inherited disorder and most common blood clotting disorder. It slightly increases your risk of deep vein thrombosis or pulmonary embolism.
- Prothrombin Gene Mutation- an inherited condition that slightly increases your risk of deep vein thrombosis or pulmonary embolism.
- Antiphospholipid Syndrome- an autoimmune disorder that increases the risk of blood clots.
People who have an increased risk of developing blood clots include:
- People 65 years of age or older
- Pregnancy
- People who are obese
- People who have cancer
- Those on birth control or hormone therapy
- Smokers
- Immobile people
Ways to reduce the risk of developing blood clots include:
- Avoid sitting for long periods
- Drinking plenty of fluids
- Changing your lifestyle
If you are experiencing any of these symptoms, you can schedule an appointment with a doctor at Jamaica Hospital Medical Center’s Ambulatory Care Center, please call (718) 206-7001. If you are experiencing an emergency, call 911.
All content of this newsletter is intended for general information purposes only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.



